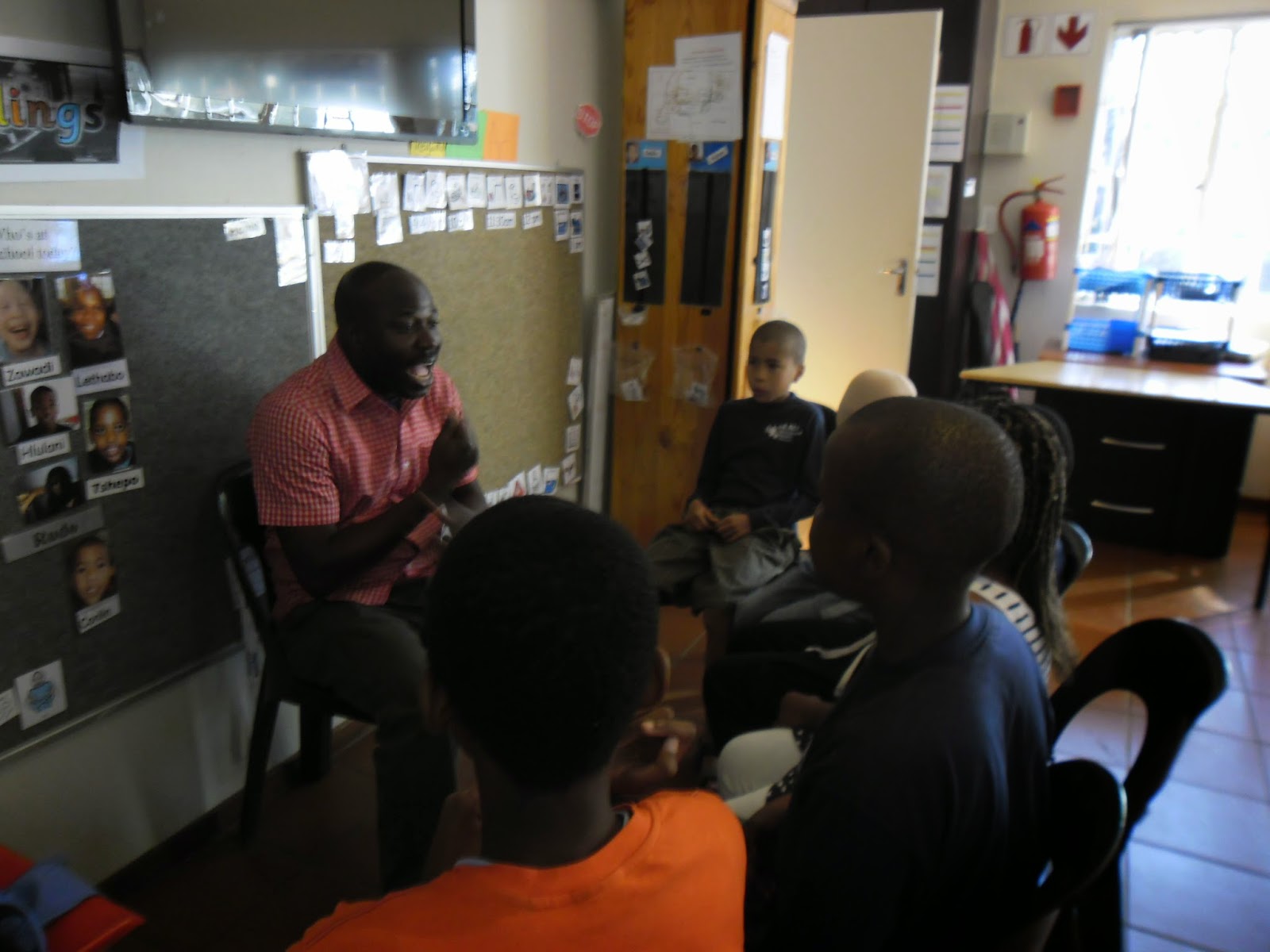
This week, Sensory Care presents to you another Therapist who is changing the world one special child at a time.
What is your name?
My name is Samuel Oluwafemi Oluwawunmi, but most of my friends call me Fesho (nickname)
Why did you choose to become a therapist?
Well, my decision to work with individuals with special needs as a therapist is a long story but suffice to say that my decision was a response to a call to serve. I had never in my wildest dreams considered this profession, not until 2006 after reading Ben Carson’s “Gifted Hands” and PROVIDENCE further confirmed that I was called as an Educator to make learning easier for individuals with special needs.
Area of interest, why?
My area of interest is definitely teaching, because I specialized in Education.
Pros of being a therapist / things you like about your vocation?
Working with these children though tough [as it requires a lot of patience both with the children and their parents] has also given me joy. For me, seeing a child learning skills he or she has never known before and also seeing their parents express satisfaction knowing that their child is able to learn is very fulfilling.
Things you dislike about your vocation?
I am so sorry to let you know that there is nothing in my vocation that I don’t love. I don’t think I would have been fulfilled doing anything else other than this.
Your happiest and saddest moments in therapy?
My happiest moment is always when I finally discover a child’s learning style or his or her most rewarding reinforcement. Because the moment you discover this, then there is no skill you cannot teach the child in any therapy session.
The moment I don’t like is when there’s no continuity at home by parents and siblings, even after they have been taught on how to work with the child and what works well with him or her.
Challenges practicing in Nigeria and or in your location?
My greatest challenges from 2006 up until February 2014 when I left Nigeria were with parents continuing from where the therapist stopped. Most of them don’t even show interest and the few who do are too busy to put it into practice because they believe the therapist should fix it.
Another challenge is with some schools who have not accepted to modify instructions, materials and assessments to suit our ASD learners. Even though I must commend some schools that are hospitable to our ASD kids, I have serious issues understanding why so many other schools have not followed suit.
Talking about modifying instructions and all, for example, tell me what is wrong when a teacher asks a child with ASD to define “a tree” and the child runs outside the class to touch a tree? Or if the child due to difficulties with fine motor cannot quickly write 1-20 on a paper but can recite offhand and identify 1-20 without any help?
Believe me, our schools need to step up and understand that knowledge expressed verbally, by writing, by gestures, or by demonstration are acceptable as knowledge.
That is the difference between a 21st century teacher/school and the 19th or 20th century schools.
The only challenge I am experiencing at the moment in the center I work in SA is with parents. The center basically provides everything without any charges yet, we have to practically beg some people to come in for their appointment or bring in recorded result.
This center is using one of the best programs for children with ASD, the Rethink Autism which is based on ABA principles but they are not availing themselves of this great opportunity to help their kids.
Favourite therapy material, why?
My favorite therapy materials are visual materials. Reason being that for people with Autism Spectrum Disorder [ASD] and some other related disorders, the preferred mode of learning is VISUAL over VERBAL.
Also if you are also talking about methods, techniques or approaches of teaching, I like the DTT (Discrete Trial Teaching) because as a teacher, an educational therapist /facilitator working with a child with SEN (esp. Autism) at home or in school environment, it makes instruction very clear to the child I am teaching. DTT involves 8 simple steps, which are:
GET THE CHILD’S ATTENTION, i.e. make sure the child is looking at you
GIVE AN INSTRUCTION OR ASK A QUESTION. Your instruction or question MUST be clear, simple and short.
E.g. Say “point to the chair” not, “Femi, can you please point to the chair.” (Please as in the case of “point to the chair” make sure no other furniture is present except the chair you want him to identify)
PROMPT/HELP/ASSIST. i.e. quickly provide assistance to help the child respond correctly to your instruction. (This is what is called the errorless way of teaching, because we know our children with ASD have the tendency to repeat errors, so it is important to prevent errors whenever possible).
REINFORCE/REWARD. i.e. give the child something he/she likes IMMEDIATELY after he/she responds (even though it’s by your help) to make them more likely to respond again independently.
FADE YOUR PROMPT/HELP. i.e. gradually provide less & less assistance each time you instruct him until the child responds independently on his own.
REINFORCE INDEPENDENT RESPONSES. i.e as the child responds with less help from you, show more enthusiasm and give him a bigger and better reward.
INTRODUCE DISTRACTOR TRIAL. i.e. once the child is responding correctly without any help at all, then introduce something else. For example, you can put a bag as a distractor and repeat the instruction “point to the chair”. A distractor must at first be something from a different category / class.
GENERALIZE. Practice your instructions in different settings, in different colors, different shapes and by different people in order to generalize the skill.
What you wish parents knew about therapy?
First and foremost, I would like parents to know that they are their child’s best therapist. If they can come to this understanding, then this will propel them to learn and understand what the OT [occupational therapist], Speech therapist, teacher etc are doing so as to use the same method/principle at home with the child. By this, everybody will be on the same page and the child’s progress will know no bounds.
Secondly, parents in getting a therapist to work with their child, above just looking for cheaper therapists, should seek for therapists who have a passion for children and upgrading their skills. They will know a therapist who has the passion to upgrade by the amount of workshops, conferences and trainings locally or internationally attended.
Thanks a lot for your time.
You're welcome.
Images courtesy: Femi







































.jpeg)






.jpeg)
.jpeg)
